New Year’s Eve brought a different kind of celebration at the Kansas Christian Home in Newton: Staff and residents received their first dose of the COVID-19 vaccine.
“We were ecstatic, absolutely thrilled that we were finally getting a step toward protecting our residents, family, friends, ourselves,” said Donna Hett, assistant director of nursing at the retirement community, where 110 residents and staff were vaccinated by a visiting team from Walgreens. “I mean we were almost dancing, we were so happy.”
Residents and staff of long-term care homes are part of the first group of people designated to receive the vaccine, along with health care workers. It’s unknown how many homes have so far received the vaccine, but all are expected to get it by the end of January.
Beginning in fall 2020, long-term care facilities across the country were invited to enroll in the government’s Pharmacy Partnership for Long-Term Care Program, overseen by the U.S. Centers for Disease Control and Prevention. The CDC engaged two retail pharmacies, CVS and Walgreens, to provide on-site vaccinations at no cost to the long-term care facilities. About 99 percent of skilled nursing facilities opted for one of the pharmacies instead of developing an alternative plan.
“This program provides end-to end management of the COVID-19 vaccination process,” said Cara Sloan-Ramos, public information officer at the Kansas Department for Aging and Disability Services. That includes storage and handling of the vaccine and reporting requirements to the government, reducing the burden on the facilities and local health departments, according to Sloan-Ramos.
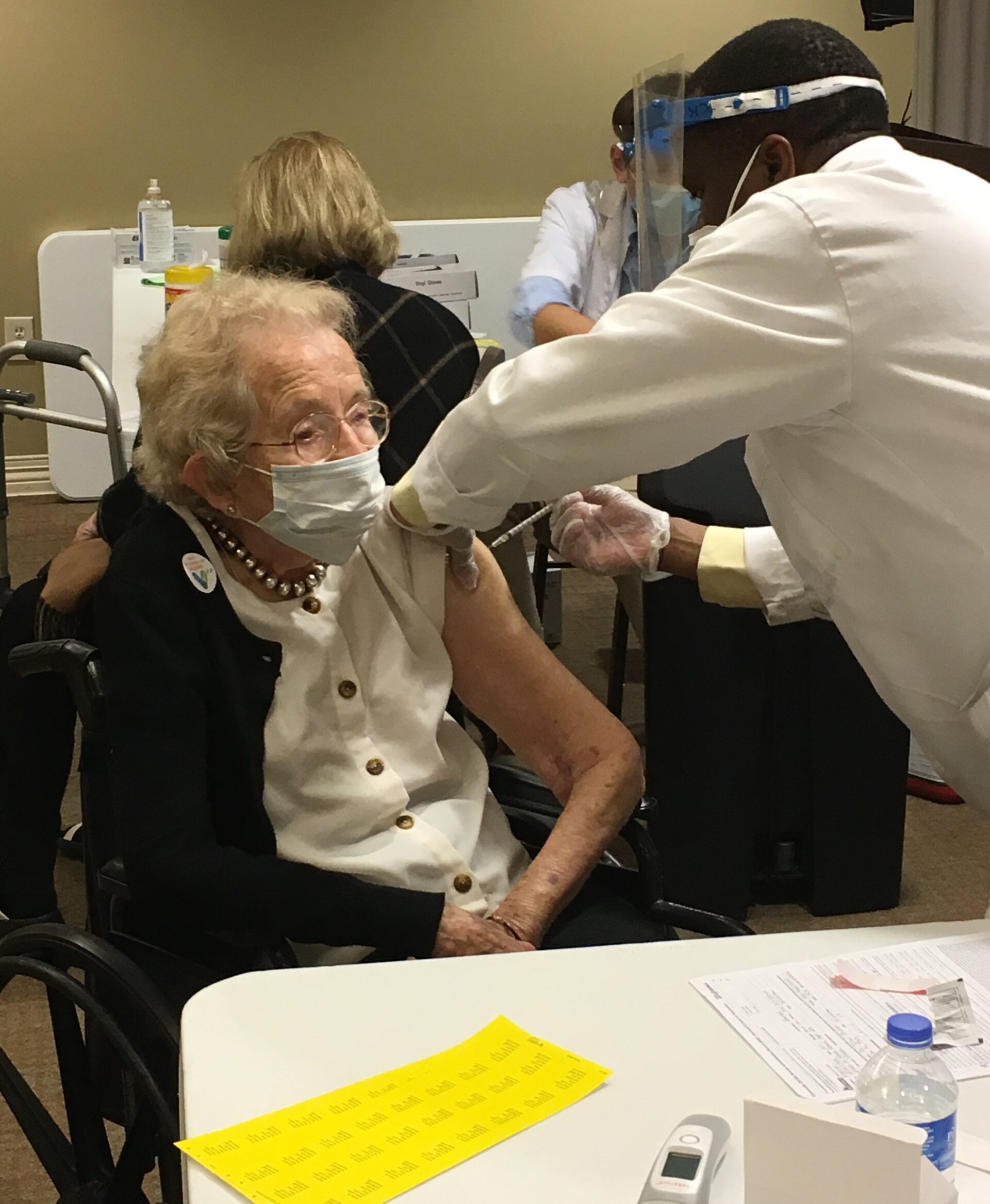
On Friday, a Walgreens team administered shots at Larksfield Place in Wichita. The day before, resident Virginia Garver said she looked forward to receiving the vaccine.
“I’m not reluctant at all and I don’t think the government would release the vaccine if it weren’t safe,” Garver said.
Garver, who’s 101, contracted polio as a toddler. She wore leg braces as a young child but suffered no long-term effects. She and her now-late husband, James Garver, reared their six children in Severy, Kan. After the children were older, she renewed her nursing license and worked as a registered nurse at Greenwood County Hospital.
Long-term care facilities constitute the deadliest category of COVID-19 clusters, partly because the virus can spread quickly in congregate living settings and older people, especially those with other health factors, are particularly vulnerable.
By Friday, 1,303 of the state’s overall 3,148 virus deaths came from the 569 long-term care facility clusters across the state.
The Centers for Medicare and Medicaid Services’ data showed that for the week ending Dec. 27, nearly 200 Medicare/Medicaid nursing homes in Kansas had reported at least one resident death from COVID-19 during the year. Over 30 of them experienced 10 or more resident deaths due to the pandemic.
The CMS data revealed the two deadliest clusters in Kansas were Garden Terrace at Overland Park, with 39 resident deaths, and Riverbend Post Acute Rehabilitation, Kansas City, with 37 residents dying.
The same database showed the highest death toll linked to the virus in Sedgwick County as of Dec. 27 was at the Catholic Care Center, Bel Aire, with 19 resident deaths. In Harvey County, Newton Presbyterian Manor had the highest, with 13 resident deaths. In Butler County, Lakepoint Augusta reported seven resident deaths from the virus in 2020.
All Kansans 65 and over are expected to qualify for the vaccine as early as February, as part of Phase 2 of the state’s vaccination plan. Prison inmates and essential workers who cannot maintain social distancing are also included in Phase 2.
Sedgwick County’s public information officer, Kate Flavin, said on Thursday that 78 percent of the COVID-19 deaths in the county have been people over age 70, and of the 136 deaths associated with a cluster category, 99 percent were linked to long-term care residents. As of Friday, Sedgwick County’s total death toll from COVID-19 was 309, and there were 70 long-term care facility clusters in the county.
Butler County Health Department Administrator Jamie Downs reported Thursday that 80 percent of the COVID-19 deaths there were people over 70, and 46 percent of Butler County’s fatalities were at long-term care facilities. Butler County had experienced 33 deaths from the virus as of Friday.
Harvey County Health Department did not supply similar data, but the county’s COVID-19 dashboard showed that at least 20 of its 29 deaths as of Friday were people age 70 or over.
Some long-term care facilities do not fall under the CMS Medicare/Medicaid umbrella and while deaths at non-CMS facilities are part of the county and state overall data, specific details about the impact of the pandemic at those sites are not available to the public in this area.
The three nursing homes reporting the most deaths in Sedgwick, Butler, and Harvey counties all experienced a surge in the fall.
Maurice Melton, 84, died from COVID-19 complications on Nov. 24 after having just been released from Ascension Via Christi-St. Francis, according to his only child, daughter Rochelle Colbert, Spring, Texas.
Melton, a resident at the Catholic Care Center, had been admitted to the hospital for two days earlier and then released. “His fever went up higher and they readmitted him,” said Colbert.
Melton suffered from mild form of dementia which worsened during his illness, Colbert said.
“Some days I still can’t believe he’s gone,” she said.
At the Kansas Christian Home, Hett described the protocol for the vaccination. The pharmacy team will return to give the second dose in the latter half of January and also will give a first dose to new residents or new hires or those who couldn’t take it or chose not to take it earlier. On the third and last visit, second doses will be given to those who need it, and some people also could get a first dose. They will have to get a second dose later from a provider.
Government does not mandate residents and staff take the vaccine.
“Forcing a person to receive the vaccine against their will would be battery, a crime, or the basis for a civil claim against the person giving the shot. It is possible but doubtful, I hope, that facilities might try to require it as a condition of continued employment,” said Margaret Farley, executive director of Kansas Advocates for Better Care. “Nursing facility staff have the rights common to all citizens: to consent or not,” she said.